Stress Fractures of the Foot and Ankle
Our bones are important aspects of our body and they are constantly changing. The heavier the workload for a bone, the more likely it is that calcium will be placed in it. When a bone isn’t used often, there won’t be much calcium within it. When stress from repetitive loads prevent the bone from being able to repair itself, cracks will start to form. Stress fractures are defined as cracks in a bone that result from repetitive force, such as overuse.
The most common cause of stress fractures is a sudden increase in intensity and duration of physical activity. For example, if you begin to run long distances without working your way into doing so, you will be more likely to develop a stress fracture.
Common symptoms of stress fractures are pain and swelling near the weight bearing area on the injured bone. When initial x-rays are performed, it is possible that the fracture will not show up. However, once the stress on the area continues, the damage will increase, and the fracture will be severe enough to show up on an x-ray. Certain parts of the foot are more likely to develop stress fractures than others. Areas that typically have these fractures are: the metatarsals, the navicular bone, the calcaneus, tibia, and fibula.
Since women are at an increased risk of developing osteoporosis, they are twice as likely as men to sustain a stress fracture. Additionally, old age causes a decrease in bone mineral density which is why elderly people are also likely to develop these fractures.
It is important for you to be professionally diagnosed by a podiatrist if you suspect you have a stress fracture, because there are other injuries that can easily be mistaken for a fracture. Sprains, strains, shin splints, plantar fasciitis, and Morton’s neuroma can all easily be mistaken for stress fractures in the foot. Your podiatrist will likely ask you a series of questions to determine what type of pain you are experiencing. These questions will help your doctor identify whether you have a stress fracture.
The best method of treatment for a stress fracture is rest. Additionally, a walking boot, cast, or crutches, will help rest the area that is injured. The typical healing time for stress fractures is 4-12 weeks, however this depends on which bone is involved.
How Did I Develop Toenail Fungus?
A noticeable sign that you may have a toenail fungus is the condition of the nails. They can become yellowed or white, and will be thicker. In severe cases, the nails are brittle and patients may find they can crumble, or fall off. The fungus that causes this condition lives and thrives in warm and moist environments, consisting of public swimming pools, communal shower room floors, and locker rooms. It is beneficial to avoid sharing towels, socks, and shoes, as this may help to stop the spread of this stubborn fungus. Additionally, wearing appropriate shoes while in these areas may protect the feet from developing toenail fungus. If you feel you have toenail fungus, it is suggested that you seek the counsel of a podiatrist who can help you to manage this condition.
For more information about treatment, contact James P. Huish, DPM of Arizona. Our doctors can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact our office located in Safford and Sierra Vista, AZ . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Treating Toenail Fungus
Fungal infection of the toenail, or onychomycosis, typically appears as a gradual change in a toenail’s texture and color that involves brittleness and darkening. The fungal infection itself occurs beneath the surface of the nail. Aside from discoloration, other symptoms include the collection of debris beneath the nail plate, white marks on the nail plate, and a foul odor emanating from the nail. If ignored, the infection can spread into other nails and the skin; in severe cases, it can hinder one’s ability to work or walk.
The toenails are particularly vulnerable to contracting infection in moist environments where people are likely to be walking barefoot, such as around swimming pools, public showers, and locker rooms. Fungal infection may also be more likely to occur in nail beds that have been injured, and sufferers of chronic diseases such as diabetes, circulatory problems, or immunodeficiency conditions are particularly prone to developing fungal nails.
Fungal nails can be primarily prevented by practicing proper hygiene and regularly examining the feet and toes. Carefully washing the feet with soap and water and thoroughly drying the feet afterwards are essential. Other tips include wearing shower shoes in public areas, changing shoes and socks daily, keeping toenails clipped at a short length, wearing breathable shoes that fit properly, wearing moisture-wicking socks, and disinfecting home pedicure tools and instruments used to cut nails.
Fungal nail treatment may vary between patients and the severity of the condition. Your podiatrist may suggest a daily routine of cleansing that spans over a period of time to ease mild infections. Over-the-counter or prescription antifungal agents may also be prescribed, including topical and/or oral medications. Debridement, or the removal of diseased nail matter and debris, may also be performed. In more severe cases, surgical treatment may be needed. In some instances, the temporary removal of the fungal nail allows for the direct application of a topical antifungal to the nail bed. In other cases, a chronically painful fungal nail that has not responded to other treatments may be permanently removed; this allows the infection to be cured and avoids the growth of a deformed nail.
What Are Common Signs of Neuropathy?
 Neuropathy may be brought upon by nerve damage and can cause serious issues for the feet if left unmonitored. This condition can be fairly common among diabetic patients, often causing a loss of feeling or numbing sensation of the feet. There are a few indicators, along with the numbing and tingling of the feet, one may look out for. Some patients may experience a throbbing, burning, or stabbing type of foot pain. Because neuropathy is caused by nerve damage, these issues can lead to changes in the size and shape of the foot. It can also be common for patients with neuropathy to develop foot ulcers. Ulcers, which are deep, open wounds, can form due to neglecting cuts or scrapes on the feet, and can often lead to infection. For professional care and an advised treatment plan, please consult with a podiatrist.
Neuropathy may be brought upon by nerve damage and can cause serious issues for the feet if left unmonitored. This condition can be fairly common among diabetic patients, often causing a loss of feeling or numbing sensation of the feet. There are a few indicators, along with the numbing and tingling of the feet, one may look out for. Some patients may experience a throbbing, burning, or stabbing type of foot pain. Because neuropathy is caused by nerve damage, these issues can lead to changes in the size and shape of the foot. It can also be common for patients with neuropathy to develop foot ulcers. Ulcers, which are deep, open wounds, can form due to neglecting cuts or scrapes on the feet, and can often lead to infection. For professional care and an advised treatment plan, please consult with a podiatrist.
Neuropathy
Neuropathy can be a potentially serious condition, especially if it is left undiagnosed. If you have any concerns that you may be experiencing nerve loss in your feet, consult with James P. Huish, DPM from Arizona. Our doctors will assess your condition and provide you with quality foot and ankle treatment for neuropathy.
What Is Neuropathy?
Neuropathy is a condition that leads to damage to the nerves in the body. Peripheral neuropathy, or neuropathy that affects your peripheral nervous system, usually occurs in the feet. Neuropathy can be triggered by a number of different causes. Such causes include diabetes, infections, cancers, disorders, and toxic substances.
Symptoms of Neuropathy Include:
- Numbness
- Sensation loss
- Prickling and tingling sensations
- Throbbing, freezing, burning pains
- Muscle weakness
Those with diabetes are at serious risk due to being unable to feel an ulcer on their feet. Diabetics usually also suffer from poor blood circulation. This can lead to the wound not healing, infections occurring, and the limb may have to be amputated.
Treatment
To treat neuropathy in the foot, podiatrists will first diagnose the cause of the neuropathy. Figuring out the underlying cause of the neuropathy will allow the podiatrist to prescribe the best treatment, whether it be caused by diabetes, toxic substance exposure, infection, etc. If the nerve has not died, then it’s possible that sensation may be able to return to the foot.
Pain medication may be issued for pain. Electrical nerve stimulation can be used to stimulate nerves. If the neuropathy is caused from pressure on the nerves, then surgery may be necessary.
If you have any questions, please feel free to contact our office located in Safford and Sierra Vista, AZ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Neuropathy
Neuropathy is the weakness, numbness, and pain in the hands and feet due to damage to the peripheral nerves. The peripheral nerves are responsible for sending information from the brain and spinal cord to the rest of your body. Causes of Neuropathy include: traumatic injuries, infections, metabolic problems, exposure to toxins, and diabetes.
Diabetes is the most common cause, with more than half of the diabetic population developing some type of neuropathy. There are several types of neuropathy and they vary based on the damage of the nerves. Mononeuropathy is classified as only one nerve being damaged. When multiple nerves are affected, it is referred as polyneuropathy. One of the types of polyneuropathy is distal symmetric polyneuropathy. It is the most common for people with diabetes and starts when the nerves furthest away from the central nervous begin to malfunction. The symptoms begin with pain and numbness in the feet and then they travel up to the legs. A rarer form of polyneuropathy is acute symmetrical peripheral neuropathy, which is a severe type that affects nerves throughout the body and is highly associated with Guillain-Barre syndrome, an autoimmune disorder that attacks the peripheral nervous system and can be fatal. Although there are many types of neuropathy, most of them share the same symptoms such as pain, extreme sensitivity to touch, lack of coordination, muscle weakness, dizziness, and digestive problems. Since neuropathy affects the nerves, those affected should be careful of burns, infection and falling, as depleted sensations disguise such ailments.
The best way to prevent neuropathy is to manage any medical conditions such as diabetes, alcoholism, or rheumatoid arthritis. Creating and managing a healthy lifestyle can also go a long way. Having a healthy diet full of fruits, vegetables, whole grains and lean protein can keep the nerves healthy. These types of food have the nutrients to prevent neuropathy. Regularly exercising can help as well, but it is best to consult with a doctor about the right amount. In addition to diet and exercise, avoiding risk factors will also prevent neuropathy. This includes repetitive motions, cramped positions, exposure to toxic chemicals, smoking and overindulging on alcohol.
Do I Have a Sprained Ankle?
 The ligaments that support the ankle are extremely important. If they become overstretched or torn, an ankle sprain may occur. There are a few common symptoms that can indicate an ankle sprain has developed including pain, soreness, swelling, bruising, and difficulty bearing weight or walking on the affected ankle. It is possible to obtain a sprained ankle if the ankle gets twisted, or if the foot rolls onto its side. While ankle sprains are typically correlated with sporting accidents, they can occur from simply taking an awkward step or tripping. As far as treating an ankle sprain, a podiatrist may suggest the use of an ankle brace or splint to help protect the ankle. Swelling may be dealt with by elevating the ankle, as well as alternating cold and warm compresses. Rest is key, so refraining from bearing weight on the affected ankle can be beneficial to the healing process. For a proper diagnosis and an advised treatment plan, please consult with a podiatrist.
The ligaments that support the ankle are extremely important. If they become overstretched or torn, an ankle sprain may occur. There are a few common symptoms that can indicate an ankle sprain has developed including pain, soreness, swelling, bruising, and difficulty bearing weight or walking on the affected ankle. It is possible to obtain a sprained ankle if the ankle gets twisted, or if the foot rolls onto its side. While ankle sprains are typically correlated with sporting accidents, they can occur from simply taking an awkward step or tripping. As far as treating an ankle sprain, a podiatrist may suggest the use of an ankle brace or splint to help protect the ankle. Swelling may be dealt with by elevating the ankle, as well as alternating cold and warm compresses. Rest is key, so refraining from bearing weight on the affected ankle can be beneficial to the healing process. For a proper diagnosis and an advised treatment plan, please consult with a podiatrist.
Although ankle sprains are common, they aren’t always minor injuries. If you need your ankle injury looked at, contact James P. Huish, DPM from Arizona. Our doctors can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains are the result of a tear in the ligaments within the ankle. These injuries may happen when you make a rapid shifting movement while your foot is planted. A less common way to sprain your ankle is when your ankle rolls inward while your foot turns outward.
What Are the Symptoms?
- Pain at the sight of the tear
- Bruising/Swelling
- Ankle area is tender to touch
- In severe cases, may hear/feel something tear
- Skin discoloration
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
In many cases, the RICE method (Rest, Ice, Compression, and Elevate) is used to treat ankle sprains. However, you should see a podiatrist to see which treatment option would work best with your injury. In severe cases, surgery may be required.
It is important to ask your doctor about rehab options after you receive treatment for your injury. Stretching, strength training, and balance exercises may help the ankle heal while also preventing further injury.
If you have any questions, please feel free to contact our office located in Safford and Sierra Vista, AZ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Ankle Sprains
Although ankle sprains may not be as serious as a broken ankle, they should be given immediate attention and care. An ankle sprain can lead to a significant amount of pain, as well as limited mobility. They are often characterized by the swelling and discoloration of the skin. This occurs when the ligaments are stretched beyond their limits.
The simple act of walking can sometimes cause a sprain, which makes ankle sprains a very common injury that can happen to anyone. They occur when the ankle twists in an awkward way or rolls over itself, causing a pop or snap in the tendons around the ankle. Some people are more at risk than others. These include athletes who continually push their bodies to the limits and also people who have previously suffered accidents to the feet, ankles, or lower legs.
Most of the time, an ankle sprain is not severe enough for hospital attention. There are many at-home treatment options available, including propping the leg up above your head to reduce blood flow and inflammation, applying ice packs to the affected area as needed, taking over-the-counter pain relievers and anti-inflammatory medication, using an ACE bandage to wrap and support the injured ankle, and most importantly, remaining off your feet until the ankle has fully healed.
Despite this, an ankle sprain can turn into a severe injury that might require hospitalization. If the ankle ligaments or muscles are damaged from a tear or rip, that is one sign that the sprain is severe enough for hospital attention and possibly for surgery. Even after the surgery, the recovery process can be long. You may need to have rehabilitation sessions administered by your podiatrist to get your ankle back to full health.
The severity of your sprain might become apparent if you are unable to stand or walk, consistent pain occurs over a prolonged period of time, swelling is much more severe than initially present, or if you start to experience tingling or numbness. These signs may indicate that your ankle sprain might actually be a broken ankle, an injury that requires immediate medical attention.
Although they are not completely avoidable, ankle sprains can be curbed with some preventative treatment measures. These include wearing appropriate-fitting shoes that not only provide a comfortable fit, but also ankle support. It is also recommended to stretch before doing any kind of physical activity, as this will help lower your body’s chance for an injury.
Why Does it Feel Like I’m Stepping on a Pebble?
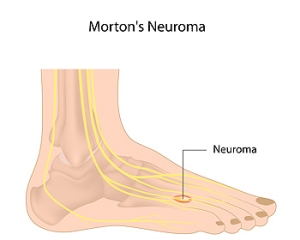
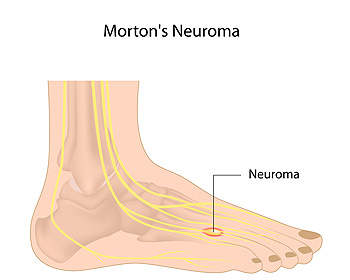 Morton’s neuroma is a condition that affects the ball of your foot. Over time the sheath surrounding the nerve becomes irritated or inflamed and forms a thickened scar tissue. The most common site of pain is between the third and fourth toes. Pain from this condition is often described as, feeling like a pebble is in your shoe and you keep stepping on it. The pain may be sharp, or you may feel a burning sensation or numbness. People who wear high heels, run regularly, or who have other foot deformities such as hammertoe, bunions, or flat feet are at an increased risk of developing Morton’s neuroma. If you are experiencing foot pain, it is suggested that you see a podiatrist, who can diagnose and treat your problem.
Morton’s neuroma is a condition that affects the ball of your foot. Over time the sheath surrounding the nerve becomes irritated or inflamed and forms a thickened scar tissue. The most common site of pain is between the third and fourth toes. Pain from this condition is often described as, feeling like a pebble is in your shoe and you keep stepping on it. The pain may be sharp, or you may feel a burning sensation or numbness. People who wear high heels, run regularly, or who have other foot deformities such as hammertoe, bunions, or flat feet are at an increased risk of developing Morton’s neuroma. If you are experiencing foot pain, it is suggested that you see a podiatrist, who can diagnose and treat your problem.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact James P. Huish, DPM of Arizona. Our doctors will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Safford and Sierra Vista, AZ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
Helping Your Heel Heal
As you get out of bed in the morning and place your feet on the floor, you feel a stabbing pain in your heel. What’s going on? It could be plantar fasciitis, an inflammation of the tissue running along the bottom of your foot. Luckily, there are ways to manage heel pain at home. Rest the foot by avoiding sports and other heavy impact activities such as running or jogging. Put an icepack under the heel for 15 minutes to reduce inflammation and swelling. Stretching your calf and foot muscles and giving yourself a soft-tissue foot massage may also help alleviate pain. While home remedies can be effective, if you find that home management techniques are not working for you, or if your pain is severe, it is recommended that you visit a podiatrist.
Many people suffer from bouts of heel pain. For more information, contact James P. Huish, DPM of Arizona. Our doctors can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Safford and Sierra Vista, AZ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.